In clinical laboratories, the accuracy of diagnostic results hinges on the performance of automated biochemistry analyzerswhich are used to measure concentrations of substances such as glucose, cholesterol, enzymes, and proteins in biological samples. Calibration is a critical process that ensures these analyzers provide precise and reliable data, which is essential for accurate diagnosis, treatment planning, and patient monitoring.
Understanding Calibration of Biochemistry Analyzers
Calibration refers to the process of configuring a biochemistry analyzer to produce results that align with known standards or reference values. It involves measuring a calibration standard or solution with a known concentration and adjusting the analyzer’s output to match the true value. This process helps correct deviations caused by instrument drift, reagent variability, or environmental factors.

Why Calibration of Biochemistry Analyzers is Important
- Ensuring Accuracy and Reliability
Calibration is the process of aligning the analyzer’s output with known reference values using standard calibration solutions. Without proper calibration, even a well-maintained analyzer may produce results that deviate from true values. Regular calibration ensures that the test results reflect the actual concentration of analytes in patient samples, thereby maintaining diagnostic accuracy and supporting effective clinical decisions using biochemistry analyzers.
- Compensating for Instrument Drift
Over time, biochemistry analyzers can experience performance drift due to various factors such as mechanical wear, temperature fluctuations, changes in light sources, or electronic noise. Calibration compensates for these changes by resetting the instrument’s measurement baseline, ensuring consistent performance across multiple tests and over extended periods.
- Consistency Across Reagent Batches
Reagents used in biochemical testing can vary slightly between manufacturing batches. These minor differences can affect the analyzer’s response, potentially leading to inconsistent results. Calibration allows laboratories to adjust for these variations, ensuring that results remain consistent even when new batches of reagents are introduced.
- Compliance with Regulatory Standards
Laboratories are subject to stringent regulatory and accreditation requirements from organizations such as CLIA, CAP, and ISO 15189. These regulations mandate regular calibration and thorough documentation to verify that instruments are operating correctly. Failure to meet these standards can lead to accreditation loss, legal liability, and compromised patient safety.
- Foundation for Quality Control
Calibration serves as the foundation for laboratory quality control. Quality control (QC) samples with known values are used to monitor the analyzer’s performance, but their effectiveness relies on accurate calibration. If calibration is incorrect, QC samples may appear to be within range even when test results are erroneous, potentially allowing inaccurate data to be reported.
- Protecting Patient Safety
Above all, calibration is about patient safety. An improperly calibrated analyzer can produce misleading results, such as underreporting blood glucose levels or overestimating liver enzyme concentrations, which can result in incorrect diagnoses or inappropriate treatments. Ensuring proper calibration helps protect patients from the consequences of misdiagnosis or delayed care.

Types of Biochemistry Analyzer Calibration
| Calibration Type | Description | When It’s Used | Key Features |
| Initial Calibration | Establishes the baseline response of the analyzer to known standards. | When a new analyzer or test is installed or initiated. | Full-range setup; uses multiple standard points. |
| Recalibration | Repeats calibration to correct performance drift or after major changes. | After maintenance, software updates, or performance issues. | Adjusts to recover accuracy; often prompted by QC failure. |
| Calibration Verification | Confirms the accuracy of a previously completed calibration. | Regular intervals or as per regulatory requirements. | Uses control materials; no new calibration curve generated. |
| Two-Point Calibration | Uses two calibrators to create a straight-line calibration curve. | For linear assays (e.g., electrolytes, simple analytes). | Simple and fast; assumes linearity. |
| Multi-Point Calibration | Uses multiple calibrator levels to establish a more complex calibration curve. | For non-linear assays (e.g., enzyme kinetics, hormones). | High accuracy; supports polynomial or exponential curve fitting. |
| Batch Calibration | Performed on analyzers that process samples in batches. | In semi-automated or batch analyzers. | Applied to the entire batch before sample analysis. |
| Continuous Calibration | Occurs in real-time or at regular intervals during routine operation. | In advanced, fully automated analyzers. | Supports high-throughput; integrates with QC programs. |
Key Steps in Calibration of Biochemistry Analyzers
The process of calibrating biochemistry analyzers involves adjusting the instrument’s measurement settings based on known standards to align its output with true analyte concentrations. Each step must be executed with precision and care to maintain data integrity.
1. Preparation of Calibration Materials
The first step involves selecting and preparing the calibration materials. These are typically commercially produced solutions containing known concentrations of specific analytes. It is vital to use materials that are traceable to international standards and stored under appropriate conditions to preserve their integrity. The calibration standards must match the assay requirements and the analyzer’s operational specifications.
2. Instrument Initialization and Warm-up
Before running any calibration, the analyzer must undergo a proper initialization or warm-up phase. This ensures that the internal systems, such as temperature regulation, optics, and fluidics, are stabilized. Skipping this step may lead to fluctuations in measurement accuracy.
3. Running the Calibration Standards
Once the analyzer is ready, the calibration standards are loaded into the instrument and processed like patient samples. The analyzer measures each standard’s response and records the signal intensity or absorbance corresponding to the known concentration. Typically, multiple standards covering the full expected range of analyte concentrations are used to generate an accurate calibration curve.
4. Generation of the Calibration Curve
Based on the responses from the standards, the analyzer’s software plots a calibration curve. This curve defines the mathematical relationship between signal intensity and analyte concentration. Common curve types include linear, polynomial, or logarithmic models, depending on the nature of the assay.
5. Adjustment and Verification
If discrepancies exist between expected and measured values, the analyzer adjusts its internal settings to fit the calibration curve accurately. After the curve is established, it must be verified by running quality control (QC) samples. These QC samples have known target values and are used to ensure the newly calibrated analyzer is producing accurate and consistent results.
6. Documentation and Recordkeeping
Every calibration event must be thoroughly documented. This includes recording the date, time, calibration materials used, lot numbers, instrument settings, and technician name. Proper documentation ensures traceability and compliance with regulatory requirements and internal quality management systems.
7. Ongoing Monitoring
Calibration is not a one-time activity. Laboratories must continuously monitor instrument performance through daily quality control checks and recalibrate the analyzer when required. Trigger points for recalibration include changes in reagent lots, instrument maintenance, unexpected QC failures, or drift in results.

Common Challenges in the Calibration of Biochemistry Analyzers
Despite advancements in automatic biochemistry analyzers, various issues can arise during calibration of biochemistry analyzers that may compromise data quality, disrupt laboratory workflows, or lead to incorrect patient results. Understanding these common challenges is the first step toward mitigating them effectively.
- Reagent and Calibrator Instability
One of the most frequent calibration challenges stems from the stability of reagents and calibration standards. Exposure to improper storage conditions, such as fluctuating temperatures or expired shelf life, can lead to the degradation of calibrators. This instability can produce inaccurate calibration curves and shift analyzer baselines, leading to skewed patient results. It is essential that calibrators are stored and handled according to the manufacturer’s guidelines to maintain their validity.
- Instrument Drift and Mechanical Wear
Over time, biochemistry analyzers are susceptible to performance drift due to component aging, optical system degradation, and mechanical wear. These subtle changes can lead to deviations in signal response, making regular calibration and preventive maintenance necessary. If drift goes unnoticed or is not corrected through recalibration, it can result in long-term inconsistencies in test results.
- Incorrect Calibration Frequency
Some laboratories either over-calibrate or under-calibrate their instruments. Over-calibration can waste resources and reduce instrument throughput, while under-calibration may lead to undetected errors in patient testing. Determining the optimal calibration frequency requires a balance based on test volume, analyzer stability, and quality control trends. Rigid adherence to outdated schedules without considering actual analyzer performance can either strain laboratory resources or compromise test accuracy.
- Human Error in Setup and Execution
Even with automated systems, human error remains a common source of calibration problems. Mistakes such as incorrect preparation of calibration standards, mislabeling, improper loading into the analyzer, or data entry errors can lead to flawed calibrations. In high-pressure or high-volume labs, these errors are more likely to occur without adequate training and verification protocols.
- Interference and Contamination
Contamination of calibration materials or carryover from previous assays can alter results and distort calibration curves. Interference from hemolysis, lipemia, or icterus in the calibration solution can also cause the analyzer to produce erroneous readings. Ensuring clean sample paths, using proper sample handling techniques, and checking for interferences are critical in minimizing such errors.
- Software or Algorithm Limitations
Sometimes, the problem lies within the analyzer’s software or calibration algorithm. A poorly selected curve fit (e.g., linear instead of polynomial), incorrect parameter settings, or software bugs can result in faulty calibration. It is important to regularly update the analyzer’s software and verify that curve fitting methods are appropriate for the specific assay.
- Reagent Lot-to-Lot Variability
Reagent formulations may vary slightly between lots, even from the same manufacturer. This variability can affect analyzer response and necessitate recalibration. If calibration is not performed when changing reagent lots, results may become inconsistent. Implementing lot-to-lot verification and performing parallel testing can help identify and adjust for such differences.

Best Practices for Effective Calibration of Biochemistry Analyzers
| Best Practice | Explanation | Benefit |
| Use Certified Calibrators | Select calibrators that are traceable to international standards. | Ensures consistency and traceability of results. |
| Follow Manufacturer’s Instructions | Adhere to recommended procedures, volumes, and timing. | Prevents procedural errors and maintains accuracy. |
| Verify Calibration with QC Samples | Run quality control samples after calibration. | Confirms that calibration was successful and effective. |
| Document Every Calibration Event | Record lot numbers, dates, personnel, and outcomes. | Supports audits, traceability, and regulatory compliance. |
| Maintain Clean Sample Paths | Prevent contamination or carryover between calibrations and samples. | Avoids errors due to residue or cross-contamination. |
| Monitor for Drift or Inconsistency | Observe trends in QC results to detect calibration drift early. | Allows timely intervention to correct errors. |
| Schedule Regular Recalibration | Calibrate periodically or based on analyzer alerts and QC trends. | Maintains long-term performance and reliability. |
| Train Staff Continuously | Ensure all users are trained in calibration techniques and troubleshooting. | Reduces human error and promotes consistent practices. |
| Use the Right Calibration Type | Choose between two-point, multi-point, or verification based on the assay. | Improves accuracy based on test complexity and behavior. |
| Inspect Reagents and Calibrators | Check expiration dates and storage conditions before use. | Prevents usage of degraded or unstable materials. |
Summary
Calibration of biochemistry analyzers is a foundational process that safeguards the accuracy and reliability of laboratory testing, which contributes to the patient safety, clinical decision-making, maintaining laboratory accreditation,etc. Through following systematic calibration practices and using high-quality standards, laboratories can ensure optimal analyzer performance.
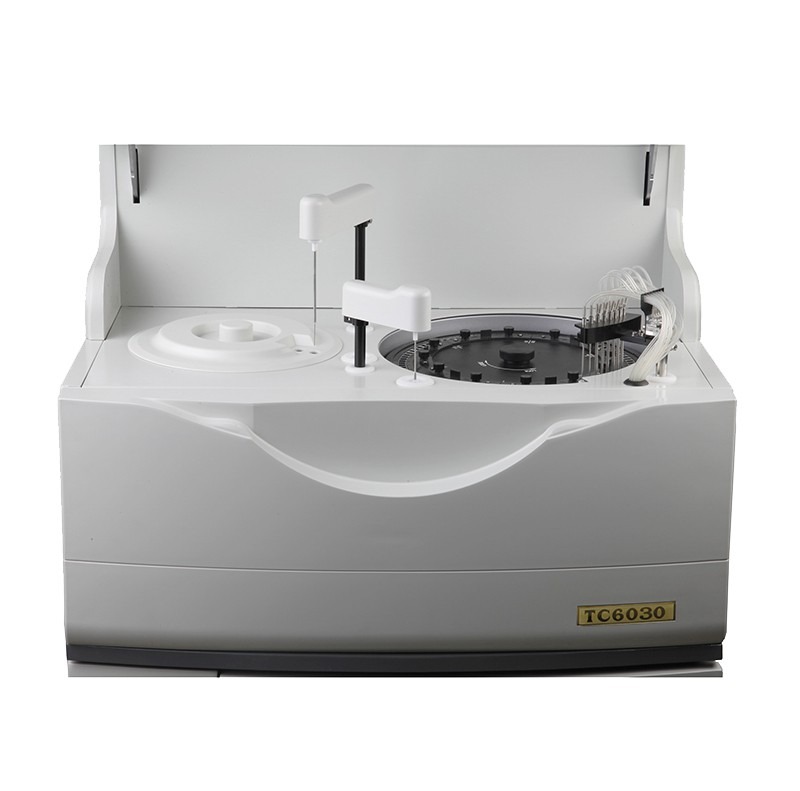
Related Products Recommendation
Get Quote Here!
Latest Posts
What Next?
For more information, or to arrange an equipment demonstration, please visit our dedicated Product Homepage or contact one of our Product Managers.