As we all know, a monitor is a medical device commonly used in disease treatment. It continuously monitors the patient’s physiological parameters during use, detects changing trends, and can alarm and remind abnormal monitoring signals to point out critical situations for doctors’ emergency treatment and treatment.

Whether it is a patient or a family member, it is very important to understand the monitor, and being able to understand the monitor will also make the patient’s companion feel more at ease and assured.
What is a monitor?
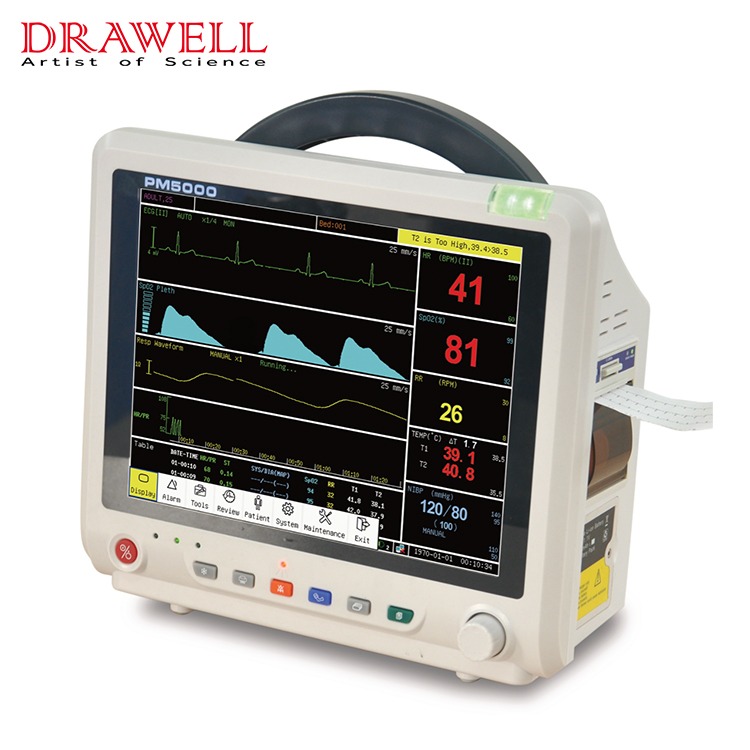
Monitors are instruments used to closely monitor and assess the condition and are mainly divided into desktop monitors and telemetry monitors.
With a telemetry monitor, the patient can walk while wearing it, mainly used for patients who need to monitor their heart rate. It can record the patient’s heartbeat rhythm in real time. If there is an abnormal heartbeat, it can be detected in time and retrospectively analyzed.
Desktop monitors can often record heart rate, blood pressure, and respiratory rate, and can also detect hypoxia by monitoring finger oxygenation.
The main application scenarios of the monitor
There are many scenarios for monitor applications, and monitor products are needed both inside and outside the hospital.
According to different clinical needs, different types of monitoring products will be used. Scenarios, where monitoring products are used, include:
1. In the hospital: emergency, outpatient, general ward, intensive care unit, operating room, in-hospital transfer, etc.
2. Outside the hospital such as home.
What are the values on the monitor?
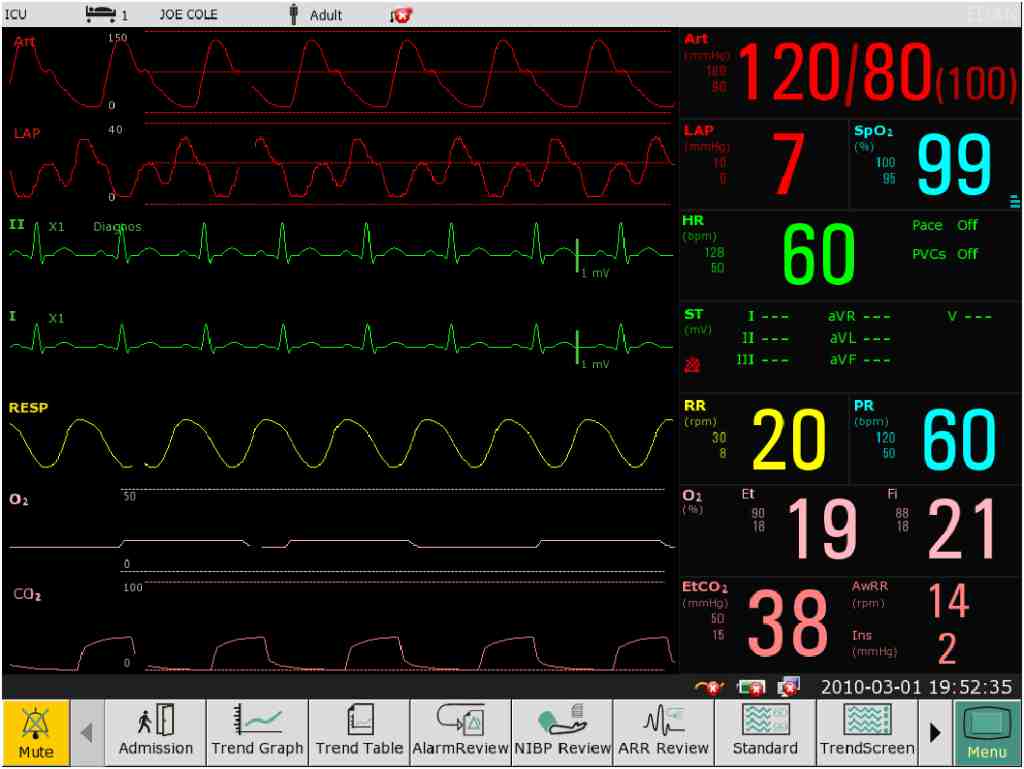
The ECG on the ECG monitor is generally an electrocardiogram, and the right side is a column of values from top to bottom. The green value represents the heart rate. NIBP is non-invasive blood pressure, which is usually called blood pressure. SpO2 is blood oxygen saturation. RR is the respiratory rate. TEMP is body temperature.
The numerical reference is as follows:
Heart rate: The average heart rate of a normal person is about 75 beats/min (between 60-90 beats/min).
Blood pressure: Blood pressure is usually measured one to two hours after surgery. The two red values on the left and right represent systolic blood pressure and diastolic blood pressure respectively. The normal range of systolic blood pressure is 90-140mmHg, and the normal range of diastolic blood pressure is 60-90mmHg.
Blood oxygen saturation: Hemoglobin in human blood needs to combine with oxygen to transport oxygen. Normal life activities in the human body require oxygen. Blood oxygen saturation represents the capacity of oxyhemoglobin in human blood, generally between 95% and 99%.
Non-invasive blood pressure: The non-invasive blood pressure monitoring adopts the Korotkoff sound detection method, and the brachial artery is blocked with an inflatable cuff. During the process of blocking the pressure drop, a series of sounds of different tones will appear. According to the tone and time, systolic and diastolic blood pressure can be judged.
During monitoring, a microphone is used as a sensor. When the pressure of the cuff is higher than the systolic pressure, the blood vessel is compressed, the blood under the cuff stops flowing, and the microphone has no signal.
When the microphone detects the first Korotkoff sound, the corresponding pressure of the cuff is systolic. Then the microphone re-measures the Korotkoff sound from the attenuated stage to the silent stage, and the corresponding pressure of the cuff is the diastolic pressure.
Body temperature: Body temperature reflects the result of the body’s metabolism and is one of the conditions for the body to carry out normal functional activities. The temperature inside the body is called “core temperature” and reflects the condition of the head or torso.
When can I stop using the monitor?
In the hospital, the desktop monitor can restrict the patient’s movement and cause some discomfort to the patient. Therefore, many patients hope to withdraw from the monitoring as soon as their condition improves slightly. is this right? When can I take off the ECG monitor?
The improvement of the disease that you see is only the improvement of the symptoms or the improvement of the surface. A physician’s assessment of disease improvement will be based on the natural history of the disease, the severity of the underlying disease, and the results of laboratory tests. The monitor can only be disabled with the consent of the doctor after all examinations have been completed.