Clinical biochemistry analyzers are indispensable tools in modern healthcare, aiding in the diagnosis, monitoring, and management of various medical conditions. These analyzers are instrumental in determining critical biochemical parameters in patient samples, such as blood and urine. In this article, we will explore the types of clinical biochemistry analyzers, focusing on fully automatic and semi-automatic biochemistry analyzers, and discuss key considerations for choosing the right one for your clinical practice.

What are the Types of Clinical Biochemistry Analyzers?
Clinical biochemistry analyzers can be divided into several categories based on various criteria, including their functionality, level of automation, and the types of tests they perform. Here are 2 common ways to divide clinical biochemistry analyzers:
Base on Level of Automation:
- Manual Analyzers: These analyzers require manual handling of samples, reagents, and test tubes. They are less automated and are often used in smaller laboratories with lower sample volumes.
- Semi-Automated Analyzers: Semi-automated analyzers automate some steps in the testing process, such as reagent mixing or sample pipetting, while other steps still require manual intervention.
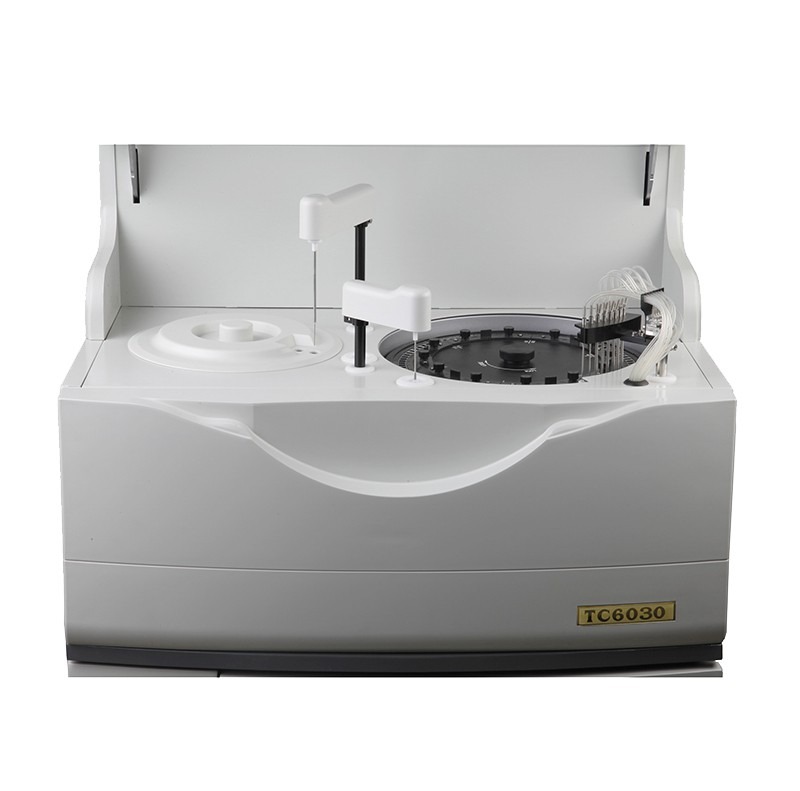
- Fully Automated Analyzers: Fully automated analyzers require minimal manual intervention and can perform a wide range of tests with high throughput. They are commonly found in large clinical laboratories.
Base on Types of Tests:
- Clinical Chemistry Analyzers: Analyzers that measure a broad range of biochemical parameters, including glucose, electrolytes, liver function, kidney function, and lipids.
- Immunoassay Analyzers: Analyzers that focus on detecting and quantifying specific proteins, hormones, antibodies, antigens, and therapeutic drugs.
- Coagulation Analyzers: Analyzers that assess blood clotting ability by measuring parameters like PT, aPTT, and INR.
- Blood Gas Analyzers: Analyzers that measure blood gases (O2, CO2) and pH in blood samples.
- Urine Analyzers: Analyzers designed for urine sample analysis, measuring parameters like pH, specific gravity, and the presence of substances like glucose, protein, and bilirubin.
- HbA1c Analyzers: Analyzers that measure glycated hemoglobin (HbA1c) levels for diabetes management.
- Enzyme Analyzers: Analyzers used to quantify specific enzymes in blood or other biological fluids.

How to Choose Clinical Biochemistry Analyzers? Fully Automatic or Semi Automatic?
Choosing between fully automatic and semi-automatic clinical biochemistry analyzers depends on several factors, including the laboratory’s specific needs, budget, sample volume, and available personnel. Here are some considerations to help you make an informed decision:
- Sample Volume: Consider the volume of samples your laboratory processes daily. Fully automatic analyzers are more suitable for high sample volumes, as they can handle a large number of tests quickly and efficiently. In contrast, semi-automatic analyzers may be sufficient for smaller laboratories with lower sample throughput.
- Test Menu: Evaluate the range of tests your laboratory needs to perform. Fully automatic analyzers typically offer a broader test menu and can run multiple tests simultaneously. If your laboratory requires a wide variety of tests, a fully automatic analyzer may be more suitable.
- Labor Resources: Assess the availability of trained laboratory personnel. Fully automatic analyzers require less hands-on intervention, making them ideal for laboratories with limited staff or a high workload. Semi-automatic analyzers require more manual steps and may be better suited for laboratories with skilled technicians who can perform the necessary tasks.
- Turnaround Time: Consider the desired turnaround time for test results. Fully automatic analyzers are faster and provide quicker results due to their high throughput and automation capabilities. If rapid results are crucial for patient care, a fully automatic analyzer may be the better choice.
- Budget: Analyzers vary in cost, with fully automatic analyzers generally being more expensive than semi-automatic ones. Assess your budget constraints and weigh the initial investment against long-term operational efficiency. Keep in mind that fully automatic analyzers may offer cost savings over time by reducing labor costs and improving efficiency.
- Space: Evaluate the available laboratory space. Fully automatic analyzers can be larger and require more space than semi-automatic ones. Ensure that you have adequate space for the chosen analyzer.
- Maintenance and Support: Consider the maintenance requirements and availability of technical support. Fully automatic analyzers may require more extensive maintenance and may have higher service and support costs. Investigate the manufacturer’s reputation for reliability and customer support.
- Integration and Data Management: Assess how well the chosen analyzer integrates with your laboratory’s existing information systems. Fully automatic analyzers often offer better data management and connectivity options, which can streamline workflow and reporting.
- Future Expansion: Think about your laboratory’s growth potential. If you anticipate an increase in sample volume and test complexity in the future, investing in a fully automatic analyzer with scalability may be a wise choice.

Conclusion
In clinical practice, the selection between fully automatic and semi-automatic biochemistry analyzers carries significant implications for laboratory efficiency and patient care. To recap, fully automatic biochemistry analyzers, renowned for their high throughput and extensive test menus, are the preferred choice for large laboratories dealing with substantial sample volumes. These advanced systems cater to facilities emphasizing speed, accuracy, and seamless connectivity.
Conversely, semi-automatic biochemistry analyzers, while less automated and requiring more manual intervention, effectively serve smaller labs, research settings, or point-of-care units. They offer flexibility, cost-efficiency, and immediate results for institutions with more modest testing requirements and skilled personnel.
Ultimately, the decision should be driven by a comprehensive evaluation of your specific clinical practice needs, encompassing sample volume, test diversity, staff expertise, budget constraints, and available resources. This thoughtful choice ensures that your clinical practice remains equipped to provide accurate diagnoses, efficient patient management, and exceptional healthcare services, contributing to the advancement of medical science and patient well-being.